There are a number of sections within this part of the document. Using the links below, or to the side, you can skip to specific sections.
- Recovery of core services
- Urgent and Emergency Care
- Elective Care
- Cancer Services
- Diagnostics
- Activity Plan
- Elective recovery
- Diagnostics
- Divisional Strategic Priorities
Jargon busting:
Despite our best efforts there may be a number of acronyms as well as NHS jargon in the our Operational Plan for 2024/25. To help, we have created this handy glossary of terms.
If you need this page in another language, please head to: https://translate.google.co.uk. For more accessibility options and information, please visit: https://www.dbth.nhs.uk/a-z/accessibility/
Recovery of core services
During 2023/24 the Trust has made significant progress in improving access to care for our patients as we continue to recover services following the pandemic. This has been despite continued periods of industrial action and increased demand for services. In particular we have:
- Improved access to urgent and emergency care, delivering the 4 hour standard in March 2024
- Reduced long waits for patients on elective care pathways
- Reducing the number of patients waiting over 62 days on a cancer pathway and delivering the faster diagnosis standard
Our overall priority for 2024/25 continues to be the recovery of our core services and productivity, to provide timely access to care for our patients. This will require a focus on improvement, reducing unwarranted variation and implementation of best practice standards such as Getting It Right First Time (GIRFT).
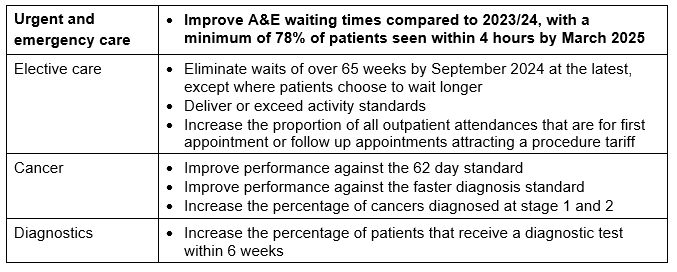
Our objectives for 2024/25 are as follows:
Urgent and Emergency Care
During 2024/25 the Trust will continue to work in collaboration with Place partners to improve access to urgent and emergency care through the delivery of a shared improvement plan. The overarching objectives are to:
- improve A&E waiting times so that a minimum of 78% of patients are admitted, discharged or transferred within 4 hours of arrival.
- reduce the number of patients waiting in A&E over 12 hours from arrival, compared to 2023/24
- improve ambulance handover times.
This will be delivered through the following key actions:
- Maintaining inpatient bed capacity at the same level as in 2023/24 to achieve bed occupancy levels required to maintain patient flow.
- Effective utilisation of the virtual ward, with a focus on frailty, acute respiratory infection and heart failure. The Trust will continue to work in partnership with community providers to develop pathways to maximise the virtual ward for patients from the emergency department, same day emergency care and inpatient wards.
- Improving admitted and non-admitted time in the emergency department through appropriate streaming at the front door, prompt initial assessment by a senior clinical decision maker and timely specialty input when required.
- Reducing the number and proportion of patients who remain in hospital beyond their discharge ready date through continued development of the transfer of care hub and timely discharge across all discharge pathways.
- Reducing the length of stay through early discharge planning, effective utilisation of the discharge lounge and a focussed, multi-disciplinary approach to longer length of stay reviews for patients remaining in hospital over 14 days.
- In collaboration with Place partners, continue to develop the discharge to assess model so that going home on pathways 0 and 1 is the default for the majority of patients.
- Reducing ambulance handover delays through prompt initial assessment at the front door, direct access to same day emergency care units and transferring patients who are ‘fit to sit’ from a trolley to a chair on arrival.
- Continued development of same day emergency care across all medical and surgical pathways, maintain services for 12 hours a day, 7 days a week as a minimum.
- Continued development of frailty services to ensure the acute frailty service is in place for at least 10 hours per day, 7 days a week.
- Ensure appropriate care plans are in place for high intensity users of A&E services so that patients can be supported to manage their needs.

Elective Care
By the end of March 2024, the Trust eliminated 104 week waits, had two patients waiting over 78 weeks and 16 patients waiting over 65 weeks. The Trust has plans in place to eliminate 65 week waits by September 2024, except where patients choose to wait longer. Recognising that the number of patients experiencing long waits cannot continue to reduce while the overall waiting list grows, the Trust will also focus on reducing the overall waiting list size.
Industrial action has had a significant impact on elective recovery; Trust plans for 2024/25 assume that there are no further periods of industrial action.
The overarching objective is to eliminate waits over 65 weeks by September 2024 at the latest, except where patients choose to wait longer.
This will be delivered through the following key actions:
- Moving procedures to the most appropriate setting and improving day case surgery so that 85% of elective surgery is provided on a day case basis through the continued implementation of GIRFT recommendations.
- Improving theatre utilisation to consistently achieve a minimum of 85% utilisation by timely pre-operative assessment and prehabilitation for patients and effective theatre planning and scheduling processes.
- Reducing waiting times to first appointment by improved clinic utilisation and reduction in ‘did not attend’ (including was not brought) rates across all specialties.
- Continued roll out of patient initiated follow up (PIFU) across all specialties, freeing up capacity for new patient appointments and reducing the backlog of follow up appointments.
- In collaboration with Place partners, increase the use of advice and guidance to avoid unnecessary referrals by the improved utilisation of the e-referral service, incorporating this into Consultant job plans.
- Improving waiting list management by the implementation of a revised Access Policy, robust operational governance processes and effective administrative, technical and clinical validation

Cancer Services
The Trust delivered the reduction in the 62 day backlog in 2023/24 and consistently delivered the 28 day Faster Diagnosis Standard (FDS) during the year.
For 2024/25, the Trust will build on these achievements with the key areas of focus as set out in the national planning guidance:
- Improving performance against the 62 day standard to 70% by March 2025
- Improving performance against the 28 day faster diagnosis standard to 77% by March 2025
- Increase the percentage of cancers diagnosed at stages 1 and 2
This will require a strong focus on pathway re-design, and on ensuring that existing and extra diagnostic capacity being introduced into the NHS is prioritised for urgent suspected cancer pathways.
This will be delivered through the following key actions:
- Making improvements in priority pathways: For example, in Lower GI, the Trust will ensure at least 80% of referrals are accompanied by a FIT (Faecal Immunochemical Test) result through the established pathways in place with primary care which are line with the British Society of Gastroenterology (BSG) / Association of Coloproctology of Great Britain and Ireland (ACPGBI guidance). Established protocols are in place within the Trust for patients referred on the Lower GI FDS pathway with FIT <10ug, FBC and normal examination, either to be discharged back to their GP or rerouted onto an alternative pathway.
- Implement sustainable breast pain pathways: Cancer Alliance funding has been utilised to explore ways to reduce pressure on the breast two week wait (2WW) clinics, and to provide an improved service to patients with Breast Pain in the Doncaster and Bassetlaw area.
- Supporting the delivery of early diagnosis programmes: for example the roll out plan for Targeted Lung Health Check (TLHC) with an update of > 53% in year and a focus on deprived areas and reducing inequalities.
- Faster diagnosis standard improvements at tumour site level: best practice timed pathways will be implemented to reduce avoidable delays in the diagnostic phase of the cancer pathway. Community Diagnostic Centre capacity will be maximised, with clear pathways and protocols, to improve access for patients on a cancer pathway.
During the Planning preparation stages, DBTH held a Cancer Priorities workshop on the 8th March 2024 where all divisions were present with the Chief Operating Officers office, Quality Improvement and Innovation, Health Inequalities and Service Development colleagues and discussed/planned in the main priorities for each division which have been captured below:

Changes Introduced
The Trust Cancer Management have introduced a number of changes around pathway management and patient support over the last 24 months whilst the ongoing issues with diagnostic capacity are addressed both locally and across the ICB.
Some of the changes are linked to process – which have been managed internally, whilst the others have allowed new roles to be developed with the support of successfully bidding for central funding to test out certain pilot projects.
Below please see a list of changes:
- Education GPs –pathways and referrals
- C the Signs tool – Primary Care
- Risk stratified follow-up pathways implementation including PIFU
- New pathways STT – Upper and Lower GI
- BPTP – Prostate, Gynaecology, ,Lung, UGI
- GIRFT recommendations – Lung
- RDS,CDC developments locally and regionally
- Additional capacity-imaging
- Additional staff-Cancer Alliance/Macmillan funded – Patient Navigators, Clinical Nurse Specialists, Advanced Clinical Practitioners, Faster Diagnosis Standard Manager, Allied Health Professionals, Pathway co-ordinators
- Prehab/Rehab pilot LGI
- Hybrid Project Support roles being developed into Medical Imaging, Dermatology and Head & Neck Services
- Clinical Harm review meetings weekly-all patients over 62 day
- Over-all for the Cancer PTL process – a minimum of twice weekly validation
- Detailed analysis and evaluation used at each step of all new developments
- Working with the wider SY&B Cancer Alliance on a Single Instance for Cancer pathways – capacity and demand function and detail next steps information
- Personalised Care progress, HNA, treatment summary’s, care plans
Moving Forward – catalyst for change
By further using guidance included within the document our next steps include:
- Specific capacity and demand and workforce planning to deliver decision to treat to treatment standard (31 day) within Dermatology service. This work will involve the guidance on the implementation of SYB single provider tele dermatology service to improve pathways.
- Support Diagnostics-pathways, protocols, increase capacity and specialist workforce across Place
- Re-visit automated day specific alerts along cancer pathways (Day 25, 35 and 50)
- Review FU systems and process-more rigor
- Understand Mandated Data requirements (FIT) and build in appropriate recording and reporting requirements. This will also provide detail reports on patient’s movement post initial telephone review
- Mutual aid-expand
- Innovation-robotics
- Support for Business case to support new pathways and additional roles
- Next steps for Governance assurance and escalation as detailed in Appendix A
- Improve on horizon scanning linked to new pathway guidelines and ensure inclusion in data forecasting the capacity required – including seasonal change and Bank Holidays.
- Increased emphasis on audit data to map, measure and improve on operational delivery. This will be on a pathway by pathway specific level.

Diagnostics
Timely access to diagnostics is critical to providing responsive, high-quality services and supporting elective recovery and early cancer diagnosis.
During 2024/25, the Trust will continue to work towards the elective care recovery plan target of 95% of patients receiving their tests within 6 weeks, individual improvement trajectories will be agreed for each diagnostic test included in the national DM01 diagnostic waiting time standard.
This will be delivered through the following key actions:
- Complete the opening and effective utilisation of all community diagnostic centre.
- Effective utilisation of i-refer for GP direct access to medical imaging to ensure appropriate requesting of tests.
- Increasing one-stop diagnostic testing and reducing waiting times from referral to report for urgent suspected cancer patients.
- Reducing non elective demand CT scans and improving compliance with national clinical guidelines.
- Reducing ‘did not attend/was not brought’ rates to improve utilisation of all diagnostic capacity.
- Reducing waiting times for Audiology services by the redesign of the service, in collaboration with Place partners.

Activity Plan
The Trusts activity plan has been developed by the clinical divisions with support from the information business partner team. Several bespoke capacity models including theatres, outpatients, endoscopy and radiology have been used as well as predictive tools to assess the impact of activity on the PTL size and long waiters. These outputs have been further refined through an assurance process with members of the Trust executive team.
To note, the Trust requested a counting and coding change from NHSE England in relation to moving IVT injections from being a daycase to an outpatient procedure. The figures below are shown before and after that change.

Elective recovery
The figures below are inclusive of the Trust’s plan to utilise the independent sector, expanded capacity from the Community Diagnostic Centres and planned productivity improvements in services. It is important to note that the 23/24 financial year included for comparative purposes was heavily impacted by industrial action and therefore the year on year step up in capacity isn’t as significant as it appears.
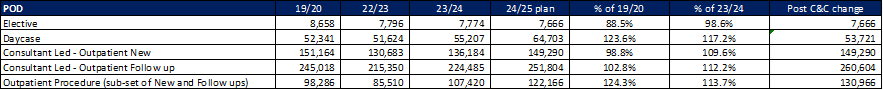
Other key points of note from the activity plans developed are:
- The increase in day case and outpatient procedures is in line with the national and GIRFT guidelines on “Right procedure, right place”
- These figures include the impact of planned work focussing on reducing “Did not attends” in outpatients, reducing on the day cancellations in theatres and moving towards GIRFT standards
Diagnostics
The Trust is planning for a significant step up in diagnostic activity in line with the national planning guidance. This year-on-year increase is mainly underpinned by the full year impact of opening additional capacity and modalities in the Community diagnostic centre.
Community Diagnostic Centre and imagine suite above in developments
The Community Diagnostic Centre (CDC) provides enhanced patient pathways and the required expansion of diagnostic services to meet expected future demand.
The CDC provided additional endoscopy lists which assisted with the recovery from COVID-19 and is now contributing to the delivery of the best practice timed pathway milestones to meet the new 28 days Faster Diagnosis Framework (FDF). The site offers new facilities, equipment and AI to assist with diagnosis.

The Montagu CDC development with its additional endoscopy provision is identified as a resource that will contribute to the developing endoscopy academy model with the potential to provide additional training capacity, and the potential to support join training posts.
Please see below for the CDC plan 2024/25:
- Increase in capacity at CDC to improve waiting times with number of additional lists as specified and utilisation of the second endoscopy room:
- 2 DBTH lists from April 2024
- 2 training lists from July 2024
- 3 ICB lists from July 2024
- 2 DBTH lists from October 2024
- Introduction of digital pathways for ICB endoscopy patients to be introduced by July 2024 with Rotherham and Barnsley
- Effective use of capacity and resources to manage pathways for other potential ICB partners
- Introduction of direct to flexible sigmoidoscopy via GP referrals through eRS
- CT/MRI independent sector vans have been used to increase diagnostic capacity via CDC routes, the static imaging unit phase of the CDC is due to be complete in March 2025. Activity will increase with the static unit as the throughput and case mix of patients increases with static machines to vanned units.
- Diagnostic activity planned to support Faster Diagnosis Standard and cancer pathways including:
- Dermoscopy imaging clinics
- Fibroscan for liver scanning
- Discussions underway to support ENT and OMFS pathways to provide additional 2ww capacity
- Review Cardio-respiratory, POCT, phlebotomy services with the plan to provide additional/ increased services at Montagu

Divisional Strategic Priorities
Are all set out in respective Division’s individual Annual Plans, main key areas of focus include:
Women and Children
- CNST Year 6 Standards/Single Delivery Plan
- Paediatric and Neonates Consultant split rota
- Achievement of British Association of Perinatal Medicine (BAPM) Nursing Standards
- Workforce recruitment and retention – Medical/Nursing/Admin
- Matching Obstetric capacity to demand – Additional 1.5 weekly lists needed for Elective Lower Segment Caesarean Section (ELSCS)
- Achieving Cancer Waiting Times
- GIRFT
- Paediatrics to Adult transition – developmentally appropriate health care
- SEND Transformation
- Achieving National KPI’s
Urgent and Emergency Care
- Rota Development – Identification and introduction of new rota system to support safe, effective and efficient workforce models across division – is part of wider corporate system.
- Staffing Levels – Review of required staffing levels and minimum standards to support safe and effective care.
- Nursing Skill Mix Review Across DRI and Bassetlaw – Skill mix review to be undertaken to determine if this can be completed within budget.
- UEC Front Door redesign – Urgent Treatment Centre (UTC) Model of Care – Introduction of model of care whereby patients enter the system via a primary care assessment to ensure the right patient, is in the right place in front of the right clinician, to allow emergency medicine to focus on higher priority patients.
- Development of new Same Day Emergency Care (SDEC) model – Development of SDEC model to support multi-specialties across UEC.
- Re-Model of Resus areas. The resuscitation room estate on the DRI site is in need of modernisation.
Medicine
- Delivery of key planning standards
- Regular transparent reporting against key metrics and related improvement plans
- Outpatients transformation – DNA rates, PIFU rates, use of virtual opportunities
- Recovery plans for key specialties where demand outstrips capacity – initial focus on dermatology, respiratory and endocrine.
- Work to identify how we can support colleagues and aim for improvement on staff survey results.
- Focus on ensuring the income to the department is correct and that contracts we hold are delivering quality and value for money
- Key staffing reviews will take place. Including but not limited to; divisional support staff, cardiology cover for pacemakers, diabetes nursing, consistency of job plans, focus on sickness reporting and rates.
- Digital; work with partners to deliver the key work streams (for example endoscopy software, cardiac MRI software) and potential new pieces of work – Dermatology EOI & Echo images
- Work with key partners to deliver changes to estates. For example; Relocation of gastro ward at BDGH, working with the CDC to develop Cardio Respiratory offer.
- Service improvements: For example; Dermoscopy and fibroscan roll out at CDC, Discharge and flow, Frailty Pathways, Length of stay, continuity of care for pacemaker patients.
- Reduce pressure ulcers and falls and increase patient engagement
- Medicine bed review – occupancy is disproportionate to other divisions
Clinical Specialities Services
- Review expansion of medical imaging capacity to meet ongoing growth in demand
- Maximising efficiency of pre-operative assessment processes and working collaboratively with surgical division to achieve this
- Agreeing strategies for non-sustainable vulnerable services – specifically critical care at Bassetlaw, Interventional radiology and several clinical therapy specialities
- Rationalisation of pain management service
- Be key enabler for enhancing patient flow and reducing length of stay, eg pharmacy robot, discharge to assess wider implementation
- Support implementation of new surgical services and Cancer Alliance Priorities
- Improve cost effectiveness and productivity – Pharmacy, Clinical Therapies, Radiology, Theatres – including review of all contracts and SLAs
- Review of Outpatient capacity
- Work with service leads to create informed workforce plans for next 3-5 years
- Minimise patient harm and report on patient experience
- Develop a 5 year plan for equipment planning for all services in line with Medical Equipment Group (MEG)
- All services to have a data dashboard to demonstrate quality and performance in line with National Benchmarking and local KPIs
Surgery
- Expand and improve elective capacity through improvement and transformation programmes for both theatres and outpatients with a focus on:
- Utilisation
- Improved Average Cases Per List
- DNA and CNA rates
- Focus best practice through GIRFT and Further Faster principles for most challenged services:
- T&O
- Ophthalmology
- Urology
- ENT
- Maximise productivity through robotic surgery, General Surgery, Urology
- Focus on supporting retention of vulnerable staff groups
- Development and implementation of sustainable Trauma business case
- Ensure the division is in line with the Trust-wide banding of ACPs to ensure parity across service
- Review expansion plans and support for ANP / ACP / AHP recruitment and retention programs- Breast, Dental, ENT, General Surgery, Ophthalmology, Trauma & Orthopaedics
- Review requirement to increase Orthopaedic consultants to provide trauma cover 52 weeks per year in job plans
- Develop and agree joint case for recruitment with Medicine to provide appropriate Geriatrician input across the surgical specialties, i.e. Trauma and Orthopaedics, General Surgery, Vascular, Urology
- Increase in Urology consultant linked to demand in service
- Explore alternative recruitment plans within Ophthalmology to bridge the clinical gap of 3 Consultant Vacancies

- Next section: People
Content out of date? Information wrong or not clear enough? Report this page.

