There are a number of sections within this part of the document. Using the links below, or to the side, you can skip to specific sections.
- Quality planning
- Clinical prioritisation
- Reducing health inequalities
- Delivering improvements in maternity care and Ockenden recommendations
Jargon busting:
Despite our best efforts there may be a number of acronyms as well as NHS jargon in the our Operational Plan for 2024/25. To help, we have created this handy glossary of terms.
If you need this page in another language, please head to: https://translate.google.co.uk/
Quality planning
In line with the NHS Operational Planning Guidance 2024/25, at DBTH we will continue to:
Maintain our focus on quality and safety of services, particularly maternity and neonatal services, and reduce Health Inequalities in line with the Core20PLUS5 approach and continue to implement the Patient Safety Incident Response Framework (PSIRF)
At DBTH, we are proud of our open, learning culture. When we identify learning, we share it, develop local action plans and ensure we are continually improving our services in response.
The Trust had a CQC inspection in 2023 of the core services Urgent and Emergency Care, Medicine, Surgery, Maternity and Diagnostic Imaging.
Following the receipt of the final CQC published report, we have developed a CQC action plan. We have taken a trust wide approach to our action planning as such there is an overarching action plan spanning all areas. The action plan will be monitored through the Trusts internal governance processes.
Successfully managing quality relies on commitment, consultation and co-operation with all staff from the ward to the Board. We will ensure the quality priorities are appropriate and meaningful to all. Data and evidence will also play a vital role; each year we will ask where is there scope for improvement and in which areas is the quality gap the greatest.
The feedback from our teams and our patients will help set core quality priorities that have an overarching impact across the organisation. The DBTH Nursing Midwifery and Allied Health Professionals Quality (NMAHP) Strategy outlines six strategic priorities, each allocated to a senior responsible officer.
The key deliverables for year one of quality strategy focus around a multifaceted approach, which encompasses several key elements:
- Patient Safety Incident Response Framework (PSIRF)
- Quality Dashboard
- Safe Staffing
- Care accreditation process
- Fundamentals of care
- Clinical Effectiveness
- Digital
- Care of our most vulnerable patients.
As part of our business planning approach for 2024/2025, each divisional plan for quality is aligned to and supported by the NMAHP quality strategy.
Workshops have been held with divisions and corporate teams to ensure the most appropriate quality areas improvement plans are included within their annual plans.
Any new schemes of projects for the trust will also have to undertake a Quality Performance Impact Assessment (QPIA) and Equality Impact Assessment (EIA) which is risk rated and when required (risk rating 8-15) approved by the Chief Nurse and Medical Director of the Trust before any scheme “goes live”. Any schemes identified as >15 risk rating are considered for approval by the Trust Board of Directors.
Also Business Cases for investment into capital or revenue must have a completed and signed off QPIA and EIA, before submission to committees for approval.
We are also keen that all initiatives undertake a Health Inequalities Assessment, which is undertaken using a locally developed health inequalities impact assessment tool.
Major quality initiatives and Quality Challenges
DBTH Nursing, Midwifery and Allied Health Professionals Quality Strategy supports the Trusts vision, ambition and planning objectives.

Clinical prioritisation
The Executive Medical Director’s team are committed to providing medical leadership and support for divisions and across the Trust to manage quality improvement priorities. Along with the key deliverables in the Quality Strategy, the Executive Medical Director is responsible for:
- Learning from mortality reviews and inquests
- Clinical prioritisation and review of long waiters to minimise harms, particularly with a health inequalities focus
- Training and development programmes for clinical leaders, new consultants and SAS doctors
- Substantive workforce plans, recruitment opportunities, retention of staff
- External peer review and service improvements
In addition, the Executive Medical Director’s Directorate will provide support to the Medical Examiner (ME) team to ensure there are systems in place to extend the scrutiny of non-coronial deaths across acute and non-acute sectors. This enables the ME team to provide independent scrutiny of all deaths occurring across Doncaster and Bassetlaw localities in compliance with the recent change in national legislation which came into effect from 1 April 2023.
The Executive Medical Directors Directorate will take the following steps to ensure outstanding patient experience:
- Support teams through governance processes to ensure clinical outcomes reflect the excellence of care provided
- Ensure medical leadership and support is provided to divisions and other departments to deliver the clinical safety and clinical effectiveness agenda to continually improve patient outcomes
- Provide support to clinical governance leads to develop their skills and knowledge in managing the patient experience agenda
- Work with the corporate nursing team and Deputy Chief Executive Officer to implement the new clinical governance framework
Using the approaches above and that of A shared commitment to quality and The NHS Patient Safety Strategy. Applying the Patient Safety Incident Response Framework (PSIRF) the following key actions from the NHS planning guidance will be undertaken:
- Completing and reviewing the NHS IMPACT self-assessment
- Ensure robust governance and reporting frameworks – aligning to NHSE – The Insightful Board guidance
- Embed a robust quality and equality impact assessment (QEIA) process within financial and operational decision-making (including CIPs)
- Improve engagement of patients and families in response to incidents and use new Learn From Patient Safety Events (LFPSE) service
- Training via NHS Patient Safety Syllabus for standardised practice
- Appointing at least 2 patient safety partners to safety-related governance committees

Reducing health inequalities
At DBTH we want to do all we can to tackle unfair health inequalities so have developed our first Tackling Health Inequalities Strategy. Aligned with national (NHS Long Term Plan, Core20PLUS5) and local (NHS SY ICB Joint Forward Plans, NHS Nottingham and Notts ICB Joint Forward Plans, Doncaster 1 Plan and Bassetlaw Place Plan) plans, the aim of our strategy is to embed the reduction of health inequalities in everything we do to ensure equitable access and excellent experience, thereby providing optimal outcomes for our patients and the communities that we serve. Below is our “plan on a page”.

To support this aim, we have been working on embedding a consideration of health inequalities into all our processes/policies across the Trust, such as business planning, and soon to include the Quality Performance Impact Assessment (QPIA) process (and within Monday.com), and the business case templates. We have also been working closely with the QI team to ensure that tackling health inequalities is included as a “lens” as part of the QI processes and are developing a health inequalities/QI toolkit to support staff when undertaking QI work that is explicitly aiming to tackle health inequalities.
In order to achieve our aim, our strategy has set out 6 priority areas of focus which include:
- Prevention – focusing on smoking cessation via the QUIT programme; alcohol and substance misuse via the development of an Alcohol Care Team (supported by SY ICB colleagues); the Core20PLUS5 priority areas of cardiovascular disease (working with our primary care partners to focus on hypertension case-finding and lipid optimisation), chronic respiratory disease, and early cancer diagnosis (supporting the Galleri-Grail pilot and Women’s Health Hubs); vaccinations via Making Every Contact Count initiatives.
- Elective care pathways / recovery – ensuring the reduction of health inequalities is embedded within elective recovery work, the access policy and initiatives to reduce DNAs supported by accurate, complete, and timely disaggregated data (broken down by, as a minimum, age, gender, ethnicity and level of deprivation (IMD score)) so the impact on health inequalities can be monitored and evidenced and targeted improvements made.
- Urgent and emergency care (UEC) pathways – ensuring the reduction of health inequalities is embedded within UEC pathways and our high intensity user group (HIUG) pathways supported by accurate, complete, and timely disaggregated data (broken down by, as a minimum, age, gender, ethnicity and level of deprivation (IMD score)) so the impact on health inequalities can be monitored and evidenced and targeted improvements made.
- Maternity and best start in life – providing support to our maternity departments to improve equity for mothers and babies from Black, Asian, Mixed and minority ethnic backgrounds and those from the most deprived areas, and improve race equality for staff from minority ethnic backgrounds.
- Children and young people (CYP) – focusing on the 5 clinical areas of focus as determined by the Core20PLUS5 for CYP (asthma, diabetes, epilepsy, oral health and mental health), we will work with our paediatric colleagues using our local insights (data and community voices) to support relevant initiatives.
- Research and innovation – ensuring the reduction of health inequalities is embedded within all research and innovation initiatives and conduct research in collaboration with partners that is explicitly targeting the reduction of health inequalities.
The 6 priority areas are underpinned by 1 base and 5 pillars. The base provides the foundation to the delivery of this strategy and refers to enhancing our communications, awareness and education of health inequalities for our people, our patients and our local communities. The 5 pillars encompass behaviours, models of practice and a general ethos/culture shift which when implemented will support all the work across all 6 priority areas. These pillars include:
- Understanding our communities – to ensure accurate, complete and timely access to population health data in conjunction with community voices to better understand the health inequalities and where to focus our action. The Information Analyst Team are working to ensure the inclusion of health inequalities data (including deprivation data – IMD) within our existing dashboards over the coming months/years. They will also ensure data relating to the NHS England’s Statement on Information on Health Inequalities is reported within our future annual reports. DBTH also has a new engagement partner, People Focused Group (PFG). We plan to continue to build relationships with PFG, who will support us to ensure the patient/public voice is incorporated into our work going forwards.
- Connecting people – to work closely with partners and build on existing relationships, networks, and trust. This will ensure work is aligned and supported and will prevent silo-working allowing health inequalities to be addressed using a whole system approach.
- Model of delivery – to move towards a more needs-led, compassionate social model of care and to use co-production to improve existing services and/or develop new services based on the needs of our communities.
- Access to and experience of services – to focus on the Core20PLUS5, ensuring targeted support is provided for the Core20 and PLUS groups, including inclusion health groups, particularly (but not exclusively) across the 5 service areas for adults and children and young people.
- Leadership and accountability – strong leadership and clear accountability and governance structures will support a culture shift and help to embed heath inequalities in everything we do, acknowledging that our staff may also be experiencing health inequalities.
To support the delivery of our strategy, we have also provided a 3-tier framework (see below). The framework outlines work that we can do to tackle health inequalities by: 1) increasing support/developing new services with a focus on prevention, 2) improving our existing services, and 3) influencing the wider determinants of health in our Anchor Institution role.
This framework will support teams, services, and divisions to guide thinking/act as a prompt for action.

We have also developed an associated action plan which outlines our planned areas of work, associated key performance indicators and anticipated timeframes for completion.
Evaluation and monitoring of performance against this strategy will be coordinated by the Health Inequalities Team, working in close partnership with relevant clinical and corporate colleagues. A five-year operational plan has been developed to accompany the strategy and will be the framework for which the monitoring process will occur. Annual delivery plans will be incorporated into the operational plan with clearly defined timescales against the actions to be taken to deliver the strategy objectives.
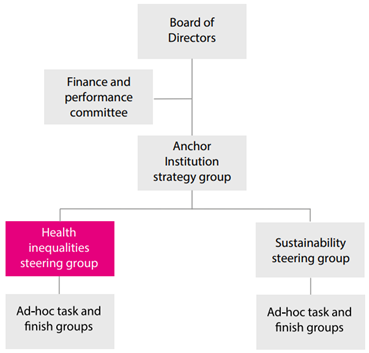
The progress of the DBTH Health Inequalities programme is monitored via quarterly reporting to the Finance and Performance Committee, with biannual updates to the Board of Directors.
The Health Inequalities and Sustainability programmes of work have come together under the umbrella of the Anchor Institution Strategy Group. There is an operational Health Inequalities Steering Group and some specific task and finish groups the latter of which will be formed to deliver the priorities outlined on a time restricted basis (see Figure below for details).
Delivering improvements in maternity care and Ockenden recommendations
In 2024/25 the maternity and neonatal service will prioritise the implementation of the three year single delivery plan, year 6 maternity (and perinatal) incentive scheme and monitor progress against the maternity self-assessment tool.
The maternity and neonatal service will continue to implement the recommendations of the three year delivery plan which include the four themes which are:
- Theme 1 – Listening and working with women and families with compassion.
- Theme 2 – Growing retaining and supporting our workforce.
- Theme 3 – Developing and sustaining a culture of safety, learning and support.
- Theme 4 – Standards and structures that underpin safer, personalised and equitable care.
This work encompasses all the recommendations from the two Ockenden reports, East Kent, the NHS long term work plan and other national maternity reports. Progress against this single delivery plan is monitored and assessed by the local maternity and neonatal system (LMNS). This consolidates the improvement actions committed to in Better Births, the NHS Long Term Plan, the Neonatal Critical Care Review, and reports of the independent investigation at Shrewsbury and Telford Hospital NHS Trust as well as the other reviews noted above.

The service will also monitor and report progress quarterly against the maternity self-Assessment tool to the maternity and neonatal quality and safety committee in the division. This tool is used to assist in improving maternity and neonatal services from requires improvement to good on CQC ratings.
The maternity and neonatal service will work towards achieving full compliance with year 6 of the maternity (and perinatal) Incentive Scheme. This includes the ten safety actions requited as listed below:
- Safety Action 1 – Using the perinatal Mortality Review tool
- Safety Action 2 – Submitting the maternity Services Data set
- Safety Action 3 – Improving transitional care
- Safety Action 4 – Ensure an effective system of clinical workforce planning
- Safety Action 5 – Ensuring an effective system for midwifery workforce planning
- Safety Action 6 – Being on track to achieve full compliance with the saving babies Lives care Bundle V3
- Safety Action 7 – Listen to women, parents and families using maternity and neonatal services and coproduce services with users
- Safety action 8 – Multidisciplinary training
- Safety Action 9 – Clear oversight in place to provide assurance to the Board on maternity and neonatal, safety and quality issues
- Safety action 10 – Reporting 100% of qualifying cases to MNSI and the Early Notification scheme
Progress against these safety actions is reported to the trust board, and monitored by the Local maternity and neonatal system.
The service will continue progress on the local maternity and neonatal Five year equity and equality action plan 2022-27. This includes work closely with the maternity and neonatal voices partnership on the following:
Care of women
- Minimising the additional risk of Covid-19 to pregnant women from global majority backgrounds and their babies
- That there are personalised care and support plans rolled out across South Yorkshire
- That trusts digital strategies include capturing information about ethnicity and postcode to make sure our services are accessible to all out communities
- Material medicine networks will be set up so that by March 2024 every woman in England with medical problems has access to specialist advice and care
- The most vulnerable groups are prioritised for implementation of continuity of carer
- Working with families and healthcare workers to increase understanding of genetic inheritance and improves access to advice
- Consider the impact culture, ethnicity and language used when investigating care
Improving health
- Improving the diabetes prevention programme
- Improving mental health services
- Providing some-free pregnancy support
- Improving breast feeding rates
Family support
- Women who have complex social factors, such as drug or alcohol abuse, migrants, asylum seekers or refuges, difficulty reading or writing English have improved access to care an support needed
- Establish community hubs in the areas of greatest need
- Address social determinants of health
The workforce
- Ensure there is improved diversity in the workforce
- Implement the Workforce race equality Standard
- Tackle discrimination and abuse
- Provide cultural competency training
The service will work closely with the local maternity and neonatal systems (South Yorkshire and Notts), regional and national networks as well as the maternity and neonatal voice partnerships to continue to improve maternity services. The service works closely with the other three trusts in South Yorkshire to ensure that equitable services are provided, and where possible work collaboratively to share resources.
The maternity and neonatal services will work together to ensure that the additional funding received from NHSE for implementation of all of the above is used in the most effective way. Ensuring that all the requirements attached to the funding are met and continue implementation of the recommendations is achieved, and working towards sustained improvement in the maternity and neonatal services.

- Next section: Finance
Content out of date? Information wrong or not clear enough? Report this page.

