Dysphagia (Swallowing Difficulties)
Swallowing difficulties may occur when there are changes to the movement or co-ordination of muscles of the face, mouth or throat. The medical term for a swallowing difficulty is dysphagia. A difficulty swallowing may result in food or drink ‘going the wrong way’ and entering the airway and/or the lungs. This is known as ‘aspiration.’ If food and drink enters the lungs this can lead to repeated chest infections and/or pneumonia. The inability to eat and drink may lead to malnutrition and dehydration. If swallowing difficulties are not appropriately managed, the consequences can be very serious.
What causes a swallowing difficulty?
A difficulty swallowing may be a result of a number of different conditions, including:
- Stroke
- Progressive neurological disorders, including
- Dementia
- Parkinson’s Disease
- Motor Neurone Disease
- Multiple Sclerosis
- Muscular Dystrophy
- Cancer, including head and neck, lung and oesophageal – See Head and Neck Cancer
- Respiratory conditions, including Chronic Obstructive Pulmonary Disease (COPD), emphysema and asthma
- Head injury
- Learning disability
- Reflux – see reflux section of Voice Service page
Signs of a swallowing difficulty
If someone is having difficulty swallowing they may show the following signs when eating/drinking:
- Coughing
- Throat clearing
- Choking
- Food/drink coming back down the nose
- Wet or gurgly voice
- Change in colour – red or blue
- Holding food/drink in the mouth for a long time
- Change in breathing
- Lot of food/drink residue in mouth after swallowing
- Food/drinks sticking in the throat or mouth
- Difficulty biting or chewing
What do we do?
Speech and Language Therapists assess how well a person’s swallow is working by looking at the muscles involved in the swallow process. This involves the person having something to eat and drink whilst a Speech Therapist has a feel of your throat (around your Adam’s apple) as you swallow.
Sometimes a different assessment is required to look at the swallowing muscles, therefore the Speech & Language therapist may refer someone for a:
- Videofluoroscopy
- Barium swallow
- Endoscopy
How are swallowing problems managed?
- Modified diet and fluids:
- Food can be modified for someone who may struggle to control/chew food in the mouth or choke on food when swallowing.
- Thickened fluids – a thickening powder can be added to drinks for someone who is unable to manage thin fluids. Thickened fluids are easier to control in the mouth and do not spill down as quickly into the throat.
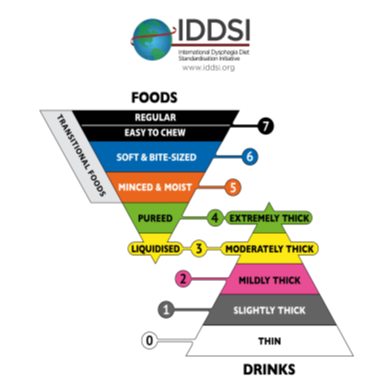
We use the International Dysphagia Diet Initiative (IDDSI) https://iddsi.org/
- Alternative feeding – at times it may be recommended that a person with swallowing difficulties requires a feeding tube. This may be to support eating and drinking or to support a person who is unable to safely eat/drink to provide main nutrition and hydration.
- Swallow exercises or techniques – specific exercises can be recommended depending on which of your swallowing muscles are affected. These can help to strengthen the muscles for swallowing, depending on the cause of the swallowing problem. Techniques may also be used to make swallowing easier and safer, again depending on the swallowing diagnosis.
How to access Speech Therapy
Inpatients Doncaster Royal Infirmary (DRI): If a patient in hospital is having difficulty with their swallowing, a referral can be made to the Speech and Language Therapy team by the ward with the doctor’s agreement. To refer an inpatient please ring 644218 and leave a voicemail. Please leave ward details, patient details and reason for referral. You can also bleep us on 1381 between 8am and 4pm.
If referring a Stroke patient call the Stroke SLT Team on 644347.
Inpatients Bassetlaw District General Hospital (BDGH): Referrals can be made by calling our DRI number 644218. Please see details above. A message will be forwarded to the SLT covering BDGH on that day.
Inpatients Mexborough Montague Hospital (MMH): The medical team are required to document in the medical notes that a swallow assessment is required. A member of the multi-disciplinary team needs to inform Speech and Language Therapy in person or phone 01709 649206.
Outpatients: If a person is having difficulty swallowing, we advise them to contact their GP who can refer to the appropriate department. This referral may be to our Speech and Language Therapy team at the hospital or it may be to a different team/profession, such as to the Community Speech and Language Therapy Team, Ear, Nose and Throat Department or Gastroenterology. We offer face to face, telephone and telehealth appointments.
If someone lives in a care home, has had a stroke, has been diagnosed with a neurological condition or is unable to attend hospital for an appointment, they will be referred to the Community Speech Therapy team provided by RDaSH and based at Tickhill Road Hospital Site.
Resources/Links
https://www.nhs.uk/conditions/swallowing-problems-dysphagia/
Back to the Adult Speech and Language Therapy Service page
Content out of date? Information wrong or not clear enough? Report this page.
